For months now since my SARPE (Surgically Assisted Rapid Palate Expansion) Surgery I have been debating sharing this video of my journey and sharing the science I followed over the last few years to cure my CFS/ME Chronic Fatigue Syndrome after 15 and a half years of suffering. This isn’t taking some magical supplement or wearing special goggles to bed, which I’m sure if you are here, you have all seen all over the internet.
This is my actual journey of battling this over the last 15 years and wanting to help those who do not have to suffer like I did because they couldn’t find answers. What got me through all this was me telling myself if what I’ve learned in the last 8 months and the procedures I went through work, I will spend the rest of my life helping people from going through the horrible years I have suffered endlessly with CFS.
I’m 44 years old, own a gym and have been training athletes for the last 22 years of my life. I own a gym with my best friend in North Scottsdale, that we have had for 12 years, and I just got my life back two weeks ago after finally feeling the benefits from opening my airway and suffering from horrible brain fog and chronic fatigue for the last 7-8 years every day. I’m not talking a little bit foggy, I’m talking I feeI like I drank a bottle of vodka before trying to drive to work some days, or I think I’m driving the wrong way in a random parking lot. This disease stole some of the best years of my life, and I thank God mine wasn’t so bad I was bed ridden.
My motivation for learning along this journey was all those I see daily on IG who can’t take care of themselves or their kids or seeing 30-year-olds living at home in bed wearing sleep masks being fed with IV’s for years now. This breaks my heart, because although this wasn’t me, many days of my life felt like this. A victim of torture that I couldn’t stop no matter how many doctors, treatments, and supplements I tried.
Many days I felt as if I had died many years ago in spirit, and my body is somehow still going but some days I thought about ending it all because I couldn’t handle another day. I lost hope somewhere along the way, and I found new depths to suffering as the months went on in life just hoping for a hail mary to get my life back. What had my life become? For someone with a job I love, a great family and friends, plenty of money in the bank, no one could help me get out of this cave. People think they know your story, but they have no clue, and it’s evident by the questions they would ask me. I would tell people I sleep all weekend and have no energy, but the next week they I would ask if I was dating anyone? I’m over here just trying to survive and make it to tomorrow and have enough energy to do fun stuff again in life, dating is like a distant 17 steps ahead of where my goals are at?
Doctor after doctor says well you look healthy to me, yet you I was dying on the inside and there isn’t a blood marker to prove it, so you I guess you just go on fighting in a cave of darkness. I have chased doctors all over the world for the last 7 years, I’ve done every test and seen pretty much any kind of doctor, and probably spent close to $200k in treatments and doctors, and my goal with this video is to just help one person if I can. The fact that I’m posting this today brings me so much joy for those that think there aren’t any answers to this, but what if there are? What if my story can help a handful of those who have lost all hope, maybe all that suffering was for a reason! This video is about sharing the science and thinking that cured me and I hope some of you watching can walk away from all this with some action steps to take to find some answers.
If you would have told me five years ago that all this is a result of having the nose of a 4-year-old and not being able to breathe through my nose, I would have laughed at you. 1,000 of hours later of podcasts, medical journal articles, and books from some of the best ENT’s, orthos, dentists, sleep docs, and functional med docs I taught myself the ABCs of airway function, why it matters, and how it’s the root for many of the disease that exists today! First of all, I would have said it’s impossible for my nose to be that small, a doctor would have realized it along the way and said something. NOPE! What I have found through all this is that many doctors live in this little tunnel, and I’m not saying all, because a few amazing doctors have been a godsend on my journey. They tend to specialize in a piece of medicine and in school weren’t given a lot of the education teaching them in all the ways the body is connected and how to spot some early signs and symptoms that might act early in life, before the effects present themselves like and avalanche and then people don’t know how to get out!
Someone I’ve been going back and forth with for a while now on IG asked me if I was sick as a kid today?
(MY RESPONSE) I was a bubble boy. Sick my whole life. Asthma and allergies were horrible as a kid. My mom told me at 3 months I would be in ER with asthma attacks. I always had colds, boatloads of antibiotics and strep throat at least once a year. I just never felt healthy and got sick my whole life. I think due to immunity I also developed celiac disease in 2009. It’s crazy to think most of this all goes back to airway health and the 200+ docs I’ve seen in my life never saying anything about it, except that I was a mouth breather which I now think of like a kid being told by a doctor that they have the early signs of cancer growing on their face, but not being told to take any action with that information!
Life is a wild ride and I’m just grateful to be sitting here today knowing that all that I’ve learned can be used to help guide others who don’t know where to start. Just reminding myself that maybe the suffering will have been well worth it someday looking back if I’m able to help others who lack the knowledge to get better. Regardless, I don’t wish this disease on anyone. When they call it a “silent disease”, I sometimes laugh, and think to myself it really is. It’s often something that you really do suffer with alone regardless of the amazing people we have in our lives.
DR AVRAM GOLD ON DR STEVEN PARK’S PODCAST: https://apple.co/3Aao3Du
A special thanks to that random podcast that I came across where Dr. Avram Gold went down with his knowledge on UARS (Upper Airway Resistance Syndrome). His explanation on how to test for it in a lab set of flags in my mind, and that wormhole saved my life. I remember walking into his lab the first night and thinking back to all the places and testing I had tried, and really asked myself “What if this is really it?” What if this is the crumb I’ve been looking for in this 15 year investigation. Nine months after meeting Dr. Gold I have gotten my mind and energy back and I’m here to share the science that got me to the finish line!
Dr. Avram Gold, Stonybrook Hospital
Best of luck on your journey and I hope this helps many people. Please share with those that maybe need help and lack the energy to find answers! I am amazed everyday by the CFS community, and the support people provide for this ungodly sickness. This disease created within me a passion to never let another soul suffer with this if I can help it! My prayers go out to all of you!
WHAT IS UARS AND HOW BEING SLEEP TESTED BY SOMEONE WHO TRULY UNDERSTANDS IT, WAS THE GAME CHANGING DISTINCTION FOR MY HEALTH!!!
UARS is defined as a subtle or partial blockage of the airway due to relaxation or partial collapse of the nasal passages or tissues of the throat. Based on many of the parameters during my time working with Dr. Avram Gold, many sleep centers will claim to know how to test for this, but do not really understand many of the distinctions UARS pathology. I have spent many hours trying to find a sleep specialist in Arizona who appears competent in their understanding of UARS, to test and interpret the data at a sufficient level and have been unsuccessful. This is concerning to me. That many people who are tested with Upper Airway Resistance Syndrome will be told they are fine, when in fact there is an issue. From all my reading it seems like the awareness isn’t there yet with many doctors and as a result the testing is lacking
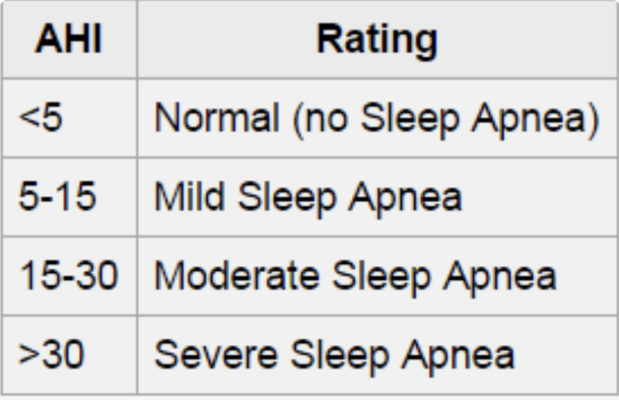
**Breathing in UARS is, characterized by an AHI below 5/hour of sleep and periods of IFL during sleep with flows greater than 50% of waking levels, terminated by arousals or changes in the background electroencephalographic rhythm associated with a return of airflow to a non-limited state. Oxyhemoglobin saturation generally remains above 90% throughout sleep. In several large studies, the mean AHI for UARS patients is consistently 2/hour, and the frequency of RERAs is between 5-20/hour.
**IFL is defined by a specific relationship of airflow driving pressure (nasal pressure minus supraglottic pressure). IFL can be more difficult to recognize in the absence of a supraglottic pressure signal because one is then missing the driving pressure; indeed, the presence of IFL can only be assumed in the absence of a supraglottic pressure tracing).
**During IFL, the ratio of the inspiratory time of the time of the entire respiratory cycle (i.e., the “duty cycle”) is prolonged. During IFL, the inspiratory airflow increases rapidly and remains near maximum throughout most of the inspiration, maximizing the tidal volume under the flow-limited conditions. During non-flow-limited breaths, the increase in inspiratory airflow is more gradual, and airflow remains maximal for a shorter portion of inspiration.
I like to call UARS the fit/thin/young man’s sleep apnea. After watching many videos from experts around the world, the biggest issue I’ve seen is that there are differing opinions on its definition and distinctions, thus making it hard to find doctors who truly understand it and are qualified to test and interpret the data.
The majority of sleep tests in-lab/at-home are designed to look for hypopneas, apneas, and desaturation. For many with UARS they do not have much desaturation and often they don’t stop breathing completely or partially for more than ten seconds which qualifies as an event during a standard sleep test. Therefore, many who fit the stereotype for this breathing pattern are often told they don’t have sleep apnea or that it’s only mild and there isn’t really an issue. Many who have UARS have a hard time breathing and work hard all night to get the job done due to smaller jaws and flimsy narrow nasal and oropharyngeal passages. The combination makes it hard to sustain breathing through the nose when the body gets into deeper levels of sleep due to the pump effect of the nasal complex being strong enough. Think of two straws: 1. A steel straw for your Yeti 32oz drink you bring to work everyday vs 2. A paper straw that is super flimsy and it got a little wet in the middle of it, making you work super-hard to get the job done.
People with UARS tend to have inspiratory airflow issues and have a hard time overcoming the negative resistance when in deeper levels of sleep. Inspiratory airflow limitation, IFL describes a state of the upper airway (the pharynx) during sleep in which the inspiratory airflow plateaus at a maximal level despite a continued increase in the pressure gradient between the nostrils and the hypopharynx. This is caused by the relaxation of the pharyngeal dilator muscles, together with the sub atmospheric upper airway pressures during inspiration. As they measure increasingly negative esophageal or supraglottic pressures during inspiratory snoring, they think of upper airway resistance increasing. The failure of inspiratory airflow to increase despite the continued pressure gradient across the upper airway is caused by fluttering of the upper airway that prevents further increase in airflow. IFL can be divided into two subgroups based on whether it is audible: (1) snoring and (2) silent IFL. What tends to happen for these patients is that when they get into deeper levels of sleep, everything gets really relaxed and the sensors in the nose and throat activate due to pressure levels and the body sensing danger. The brain which was experiencing Delta (relaxed brain waves) gets high-jacked when it senses danger, called Alpha-Delta sleep. When this happens the body downshifts from deep sleep into a lower level of sleep, only to have it hijacked later when it gets back to a deeper level of sleep again. This cycle tends to continue all night long. People wake feeling unrefreshed or fatigued, even if they slept for 8 hours. They are robbed of getting the necessary time spent in deep sleep every night to feel refreshed and mentally sharp.
These people don’t have a lack of oxygen like someone with OSA, its more that the brain waves are overstimulated from being woken up all night long. As someone who’s lived with it, it’s like being tortured every night and knowing it’s going to keep happening, but you can’t stop it. This causes a low-grade chronic state of stress. You are constantly in “fight or flight” response as a result. Then all your senses become heightened, and you are easily aroused. Common side effects are: anxiety, depression, fatigue, headaches, migraines, TMJ joint pain, teeth grinding, digestive issues, hormonal imbalances, cold extremities, normal or low blood pressure, and reproductive issues with performance as well getting pregnant. This sleep cycle reminds me conceptually like a skittish dog from the pound that has been abused. My entire life I felt like this was my nervous system.
When it comes to testing, the most critical component for someone with UARS according to Dr. Avram Gold is that you need to be measuring pressure at the nose and mouth via a pressure transducer. I was tested in a lab and titrated for a CPAP which I used for months with no effect whatsoever because the center I had gone to did not know how to recognize inspiratory airflow when they saw it. Then I flew across the country to see Dr. Gold after catching this important fact in a podcast and it changed my life. The lab in AZ told me I had mild apnea and set my CPAP pressures from 8-14. Dr. Gold evaluated me and told me that I had severe apnea when I got into REM sleep and optimal pressures for UARS is 4-9. After 2 weeks of using the CPAP after getting the right pressures, all my fatigue had gone away. It was crazy. I had messaged my doc in AZ and asked if he knew how to test for UARS, in which case he said yes. I just had to laugh. I then emailed the following criteria to the 10 best yelp reviewed sleep docs in AZ to see if I could find someone in AZ and not one person emailed me back. Just remember doctors can only test you for what they know exists and their deep understanding of said knowledge. Most sleep docs are great at identifying OSA, but when it comes to UARS doing your homework is critical!
TESTING:
In order to really recognize inspiratory airflow limitation during sleep you need to be measuring two things:
- You need to be measuring pressure at the nose and the mouth w a pressure transducer (this gives you a quality reading on the inspiratory airflow)
- You need to be able to recognize inspiratory airflow when you see it
** A word of caution- Many professionals in the sleep field don’t use an air pressure transducer to measure this. Many tend to use heat sensitive probes (aka Thermacouples) to measure inspiratory airflow limitation and this method isn’t very good at evaluating this which is a huge problem for anyone who goes to see these docs and their evaluation doesn’t pick up on this for a patient. And even if they do use a pressure transducer, they often are looking for apneas or hypopneas, and can’t read the data truly evaluating inspiratory airflow limitations w efficiency!
Three places in the US that I’m aware of that they know how to properly test at is:
- Dr. Avram Gold Stonybrook Hospital
- Dave Raapaport NY University
- Dr. Jerald Simmons in Texas
- Dr. Vik Veer in London
Common Signs/Symptoms UARS:
- Young- fit, thin or moderate weight male/females
- High narrow arched upper palates
- Tend to have normal to low blood pressure
- Mouth breathers
- Cold hands/feet
- Hypermobile at the joints (Marfan’s Syndrome)
- May have issues with Anxiety, Insomnia, fatigue
- Had 4/8 teeth pulled during childhood, left with small jaws
- May have issues with blacking out, fainting, dizziness
- Often have had issues with allergies, asthma, sinusitis
- Easily Startled
- Not breast fed, high arched narrow palat
Functional Somatic Syndromes: 2-4 times higher in females than men
- Chronic Fatigue Syndrome/ ME (Myalgic Encephalomyelitis)
- Fibromyalgia
- Chronic Widespread Pain
- TMJ Disorder
- IBS (irritable bowel syndrome)
- Insomnia
- Atypical Face Pain
- Tension Headaches
- Irritable Bladder Syndrome
- Non-cardiac Chest Pain
- Dizziness
- Chronic Low Back Pain and/or Neck Pain
- Restless Leg Syndrome
The research characterizing pharyngeal collapsibility using the critical pressure (Pcrit) has (decreasing Pcrit), there is a decrease in apnea/hypopnea index, and a shift from a predominance of apnea to a predominance of hypopnea in disordered breathing events.
The neural sensitization paradigm postulates that SDB stimulates the limbic system through the effect of sub atmospheric pressure in the nasal airway on the olfactory nerve.
**During periods of inspiratory airflow, the pressure drops between the nares and the nasopharynx, thereby creating a driving pressure
During the period of non-flow-limited breathing, the increase in inspiratory flow is more gradual and inspiratory flows are greater (nasal pressure decreases more) but the period of inspiration is shorter and the limited breathing, maximal inspiratory airflow is not as great (nasal pressure does not fall as much), but inspiratory airflow increases more rapidly and the period of inspiration is longer, exposing the olfactory nerve to longer periods of sub atmospheric pressure. The prolonged negative nasal pressure can be sensed by the olfactory nerve and transmitted to the limbic system.
THE PERFECT STORM- Snoring or silent snoring already exists, and then: Virus/bacteria/sickness, TBI, stressful event, accident, physical/emotional trauma, surgery, allergic reaction, PTSD (The olfactory nerve has a direct connection to the limbic system)
The olfactory nerve is directly connected to the limbic system—the emotional center of the brain—and senses not only smells but air pressure. Gold suspects that UARS patient’s limbic systems have come to associate a drop in air pressure during sleep with danger. For this connection to form, he postulates, there has to be a stressful sensitizing event, whether the trauma of war or sickness. And perhaps you need someone who’s more reactive to stress.
When it comes to sleep it’s not about the number of arousals someone is having, its more about the severity of their symptoms during the day. If your brain is responding to the sleep-disordered breathing as a danger, and your fight or flight systems turns on and the anxiety syndromes start up, it doesn’t matter how many times an hour you’re waking up.
Dr. Avram Gold suspects: UARS patients’ limbic systems have come to associate a drop in pressure during sleep as danger. People get sensitized during an event or stressful period in their life, perhaps these people are more reactive to stress to begin with.
*The event activates the “Hypothalamic Pituitary Adrenal Axis” and then the brain gets sensitized to snoring, aka the event or stressor.
*These people snored before (whether audible or silent) said event but following the incident they changed their relationship to snoring and it becomes a threat to them.
*When we experience a threat in life, the brain records a memory in the hippocampus that if it’s no big deal. Dr. Gold believes if there was an event or trauma that set off the limbic system it recognized snoring that someone was already doing as a threat in the hippocampus and it keeps holding onto it like it’s a THREAT, and it’s not giving up the sensitization
*The snoring now registered as a threat, when it persists, creates a cycle of chronic stress in the body where we often see issues start with the nervous system as well as the immune system. Left untreated and this can cause a plethora of chronic health issues or functional somatic syndromes which will change your life, sometimes forever!
Fix: If using a cpap or surgery for a while, the HP Axis will no longer react to snoring, cortisol levels will drop, sleep will deepen, the entire “FIGHT OR FLIGHT” response will calm down. This lets the body normalize.
The Chronic Stress Paradigm builds on the sleep quality paradigm of UARS and provides a more complete explanation of the varied symptoms associated with the syndrome.
The paradigm postulates that some individuals can become sensitized to upper airway resistance as a stimulus that activates the stress response (activation of the hypothalamic-pituitary-adrenal axis and sympathetic nervous system by the brain’s limbic system) as if it were an existential threat. Because upper airway resistance during sleep occurs for at least several hours daily, in these individuals, it constitutes a chronic stress with associated symptoms including sleep onset and sleep maintenance insomnia, headaches, gastrointestinal and bladder irritability, body pain, anxiety and depression. In addition to these symptoms, some prevalent among UARS patients, chronic stress is associated with hypertension, type 2 diabetes mellitius, gonadotrophic hormone deficiency leading to sexual dysfunction (erectile dysfunction in men and polycystic ovarian syndrome in women), and growth hormone deficiency leading to diminished growth in children. These are all prominent medical conditions associated with OSA. According to such a chronic stress paradigm, the sleep fragmentation by arousals and altered sleep quality caused by alpha frequency intrusion and a direct effect of upper airway resistance on sleep continuity, but an adaptive response of the brain to the existence of a disturbance or threat. Having sleep continuously interrupted or having a state of vigilance maintained during sleep through alpha frequency intrusion and sleep stage instability theoretically enables the individual to respond more quickly to a danger, an apparent survival advantage. This advantage, however, is accompanied by the disadvantage of parasomnias and daytime sleepiness resulting from chronically altered sleep.
**The sleep of UARS patients has the presence of RERAs and electroencephalographic differences in sleep architecture that distinguish it from the sleep of healthy individuals and also those who present with your typical OSA pathophysiologic paradigm of sleep fragmentation by apnea, hypopneas, and RERAs.
UARS vs OSA
Among this group, as the apnea/hypopnea index increases, the prevalence of Functional Somatic Syndromes tends to decrease for those with UARS. For patients with FSS and anxiety disorders, the apnea/hypopnea index from normal sleep testing without a good observation of IFL tends to be low. In one study with 18 Fibromyalgia patients who underwent polysom, the mean apnea/hypopnea index was 2.4/hour, compared to the 18 GWI participants who present more like those who traditional sleep testing was designed for had a mean of 18/hour. The research characterizing pharyngeal collapsibility using the critical pressure (Pcrit) has demonstrated that with decreasing pharyngeal collapsibility (decreasing Pcrit) like those with UARS, there is a decrease in apnea/hypopnea index. With a shift from a predominance of hypopnea in disordered breathing events.
Please message me with any questions you may have at @projectairway on IG if I can be of any help!
Greg
DISCLAIMER:
This information is not intended as a substitute for professional medical or dental advice, diagnosis, or treatment. Always seek professional medical advice from your dentist, or other qualified healthcare provider with any questions you may have regarding a medical condition. This information is not intended to diagnose, treat or cure any disease. Significant changes in your health regime should be discussed with your healthcare provider. We make no warranty, representation, or guarantee regarding the advice given here, nor do we assume any liability whatsoever arising out of your use of any information provided here.



